Rural hospitals fight same battles as in early stages of pandemic
Published 2:00 pm Wednesday, July 22, 2020

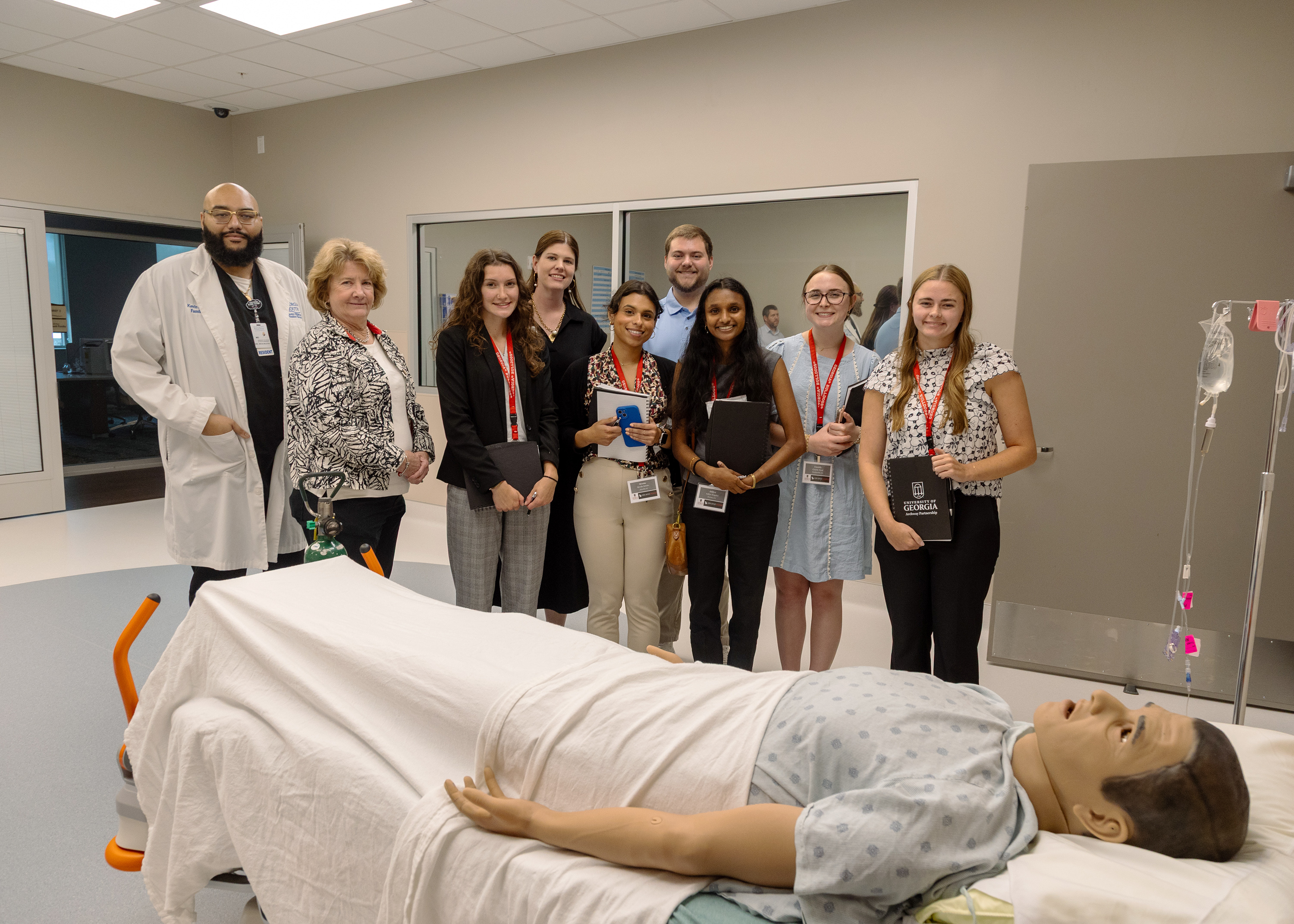
- A hospital employee straightens a room in Evans Memorial Hospital on March 5.
COLQUITT, Ga. — Robin Rau doesn’t think things will ever go back to the way they were.
Rau, CEO of the Miller County Hospital Authority, expects after COVID-19, health care systems will have to take on COVID-20 and COVID-21, or whatever coming years may bring.
“I’d like to think that we get back to prior existence, but unfortunately I just don’t see it,” she said. “It is just going to morph into something different but it’s the world that we live in right now.”
Rural hospitals in Georgia were already treading water before the pandemic hit. Facilities that were spared from early clusters watched as places like Dougherty County were overrun with positive patients.
Angela Ammons, CEO Clinch Memorial Hospital in Homerville, likened the outbreak in Albany to “watching a burning building.”
There was nothing they could do, she said, but surveying early outbreaks helped them prepare.
“We went into survival mode,” Ammons said.
The state’s rural hospitals doubled-down patient screening and disinfecting measures as elective procedures were halted — freezing millions in income — and their regular PPE providers began to reject orders.
“We realized very early on that, that we were not going to get the supplies that we asked for from our usual providers,” she said. “If I knew that it was going to impact this so greatly I probably would order more supplies. But then again, with our cash flow we’re very limited.”
Now, nearly a half year into the pandemic, rural hospitals still struggle with the same problems they faced in the first weeks — a dash to find PPE, lagging testing results and attempts to bring back outpatients for elective procedures to keep their finances intact.
Administrators of the state’s neediest hospitals have had to face the reality that COVID-19 may be a forever problem.
Treasure hunt for PPE
During the course of two days, Damien Scott, CEO of the Emanuel Medical Center, contacted 20 different medical supply vendors in search of one that could fill an order for masks. The medical facility was looking for 3,000 — a small number compared to large hospital orders — but the CEO couldn’t find any.
“Our normal supply chain will not let you order more than what you ordered to pre-COVID,” he said. “That’s when we needed like 1% of what we’re ordering now.”
Scott said every day is an ongoing search for PPE for his hospital in Swainsboro. While the state is distributing supplies across Georgia, he said, hospitals are never sure what they are going to get until the distribution.
“We came up with a plan about three weeks ago that we were going to stockpile 60 days with PPE,” Scott said. “Well that’s all good and well, if you can get it. Then what made it even more challenging as we started getting PPE, is we started also getting a pretty significant increase in patients. So we are burning through it faster.”
Emanuel County went from May 1 to June 5 without any cases — causing health care administrators to suspect the pandemic may bypass their facilities.
“I know it sounds silly saying that now,” Scott said. But the hospital was testing residents, without a single positive result for five weeks.
Now, the county has 267 cases, which most have occurred in the last few weeks. Scott said the facility is seeing increased hospitalizations.
Ammons said if she had suspected that COVID-19 would have such a serious impact, she would have ordered more supplies form the beginning. The hospital in Homerville has relied on Georgia Emergency Management Agency distributions and help from the community.
“I was one of those people saying ‘this is just a huge media hype, 30 days and it will be all over,’” Ammons said. “Now, I think this is like the mother-in-law that you’re not going to get rid of, and you just need to learn to live with.”
As of July 13, according to Clinch Memorial, the hospital had tested a little more than 1,500 patients and recorded 200 positive results.
Testing back to where it began
Time and time again, Gov. Brian Kemp and his top health officials have expressed frustration with the state’s testing capacity. In the early stages of the pandemic, testing kits were hard to find and results from both public and private labs could take weeks to get.
During the most recent COVID-19 update from the governor and responding agencies, Dr. Kathleen Toomey, commissioner of the department of public health, said the state is still working to expedite and improve the testing system.
“We also recognized the lab capacity needs to be improved, many of the commercial labs are not returning tests in a timely way, it takes as long as two weeks or longer to get a test back,” she said. “That delay is not acceptable — unacceptable both for the individual infected but also for us to do the prevention interventions to protect the public.”
Rau, who runs the facility in Colquitt, said the state is back to exactly where it started with the pandemic in terms of testing and attributes it to the “poor behavior” of young adults, bucking social distancing measures and spreading the virus unknowingly. Rau said she is seeing renewed cases in younger Georgians.
The hospital CEO said in March she had been hopeful COVID-19 would be under control by summer. But after seeing how Georgia and the country as a whole is acting — refusing masks and quickly returning to life as it was before the pandemic — she had a “sinking feeling” that her staff would be battling the virus for months to come.
As of July 17, Miller County Hospital has tested more than 1,600 patients from Miller and various surrounding counties and recorded more than 130 positive cases.
“Where the original problem when we all began this is that it took four, five, six, seven days to get a result back because there weren’t enough labs and tests available — now there’s more labs and tests available, but they are now becoming overwhelmed,” she said.
The challenges seem insurmountable. Rural hospitals are seeing increasing hospitalizations — a trend on line with a startling spike across the state — but larger hospitals are starting to refuse to accept COVID-19 patient transfers from them.
“These rural hospitals are so pressed for staff and for beds,” Rau said. “It’s almost as though you cannot overcome this.”